HEAD & Neck
A paradox exists with this section. So many conditions amenable to mechanical drainage of non vascular edema occur here but there are only a few movements or loading strategies that can be performed.
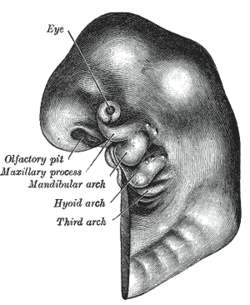
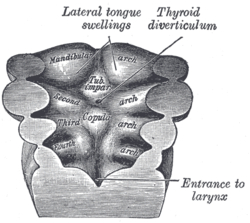
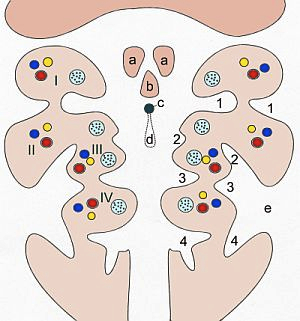
Having a basic understanding of the developing head and neck is crucial in correctly assessing and effectively treating issues arising from the area. Knowing the origins of the branchial arches, dorsal aortae and aortic sac lead to a solid anatomical and physiological base of knowledge. Knowing what nerves and cartilage are associated with the arches is of equal importance. For example, realizing structures within the petrotympanic fissure can be affected by manual therapy techniques which in turn may result in a change of blood flow within the middle and inner ear may help a tinnitus problem. Understanding the origins of the nervous system from neurulation to neuronal migration will explain the relationships between the central nervous system, the cranial nerves, and the autonomics, Being aware the sympathetics are recurrent and travel back to the brain from the upper thoracic spinal cord is critical. Correcting a forward head posture will no doubt change hemodynamics within the cranial vault.
One has to discern the following: is the presenting condition of this pathophysiology, is this a red flag condition, if it is hypoxia then what is the epidemiology (osteonecrosis?, insufficiency fracture?, enthesopathy?), how do I test for it (am I targeting the correct tissues?), what outcomes am I looking for?
Obviously not every case has this type of disability. Focal dystonias or vertebral fixations are two examples. Some cases may partially have this etiology, upper crossed syndromes (forward head postures) for example.
The patient may be presenting with a red flag. If the symptoms are of recent onset, getting worse and are not position dependent…be careful!
Restrictions of the cervical spine of the pathologic etiology contraindicate manual therapy; patients affected should be referred to relevant medical specialists. therefore, all patients must be examined prior to and continuously monitored during treatment of the cervical spine, least any existing pathological condition be worsened, increasing the risk of injury.
Prior to treatment: Assure, by test or test report, that De Kleyn’s, Hautand’s and Romberg’s tests are negative. Positive tests contraindicate manual therapy. Pathological hypermobility in a segment contraindicates stretching of that segment.
During treatment: Patient dizziness, nausea, radiating pain, or other severe discomfort during treatment may be signs of vascular spasm, anomalous blood vessels, fractures, ruptured ligaments, instability, herniated discs, or other pathological conditions that contraindicate manual therapy. The patient should be continuously monitored for these signs: If they appear, therapy should be stopped immediately.
Epidemiology and hypothesis testing play major roles in the assessment. Suppose the patient presents with chronic bilateral hand numbness. What’s the likelihood of the problem being carpal tunnel, or cervical disc, or pec minor syndrome? The history will give clues and epidemiology will give probabilities. Start testing for the most likely hypothesis.
When you do start the testing how can you tell the overpressure is applied to the correct tissue? One positive sign is the symptoms are reproduced as the overpressure is being applied. A second sign is the end range of motion has increased.
The response can be immediate or take a couple of days. It can go in 4 directions: better, somewhat or only temporary better, no change, or aggravated. It should be evident that these procedures are really orthopaedic and neurological tests. Your direction of therapy will be determined by the results of these tests. If the patient is better they probably only need to be seen 1 or 2 times. Partial results will mean you are on the right tract but will have to perform more similar tests. If no change results then reassess, and if the condition worsens consider referring out.
As a rule I perform each procedure several times during a session. I start gently and then repeat with a mild increase of force until just before I reach the end of the patient’s tolerance level. I always explain to the patient what I am about to do and get verbal consent. During each procedure I ask how the patient is doing and insist they give constant feedback. On repeating the procedure I ask for consent again, and again, and again.
The biggest factor to a successful and safe session is the patient’s feedback. After all, he/she is really the only one who knows where the problem is, if you are affecting the correct area, if there is an improvement and most importantly, if it’s causing pain or harm.
A polysomnographic study of sleep disruptions in individuals with chronic neck pain
The vestibulosympathetic reflex in humans: neural interactions between cardiovascular reflexes
Relationship between orthostatic hypotension and recurrence of benign paroxysmal positional vertigo